Intensive Care
Advancing early assessment of energy expenditure and optimal nutritional provision for improved recovery in critically ill patients in the intensive care unit (ICU).
Critically ill pateints in the ICU for more than 48 hours should be considered at risk for malnutrition.1 Those with critical illness, undergoing surgery and elderly patients are particularly at high risk.3,4 Protein is an essential nutrient for maintaining muscle synthesis and avoiding muscle degradation1 and is considered the most important macronutrient for healing wounds and maintaining lean body mass.5 Hospitalized patients including elderly, burn victims, or those with multiple trauma need markedly higher protein intake than healthy people to maintain body mass and function.2

Malnutrition is very frequent in the ICU and has severe detrimental effects
Due to the potentially severe consequences of malnutrition, it is recommended that all critically ill patients admitted to hospital are screened for nutritional risk.1 However, it is estimated that only half of malnourished patients are recognized in routine clinical practice,7 and sarcopenia often goes unnoticed.8 Sarcopenia increases the risk of complications and infections and may lead to prolonged hospitalization, permanent injury or even death.9,10
~60%
of critically ill patients already have generalized muscle loss when admitted to the ICU9
~50%
of the required protein intake is not delivered to most patients during their first week in the ICU11,12
~1 kg
of muscle mass is lost a day in critically ill adult patients during their first 5 days of ICU stay13
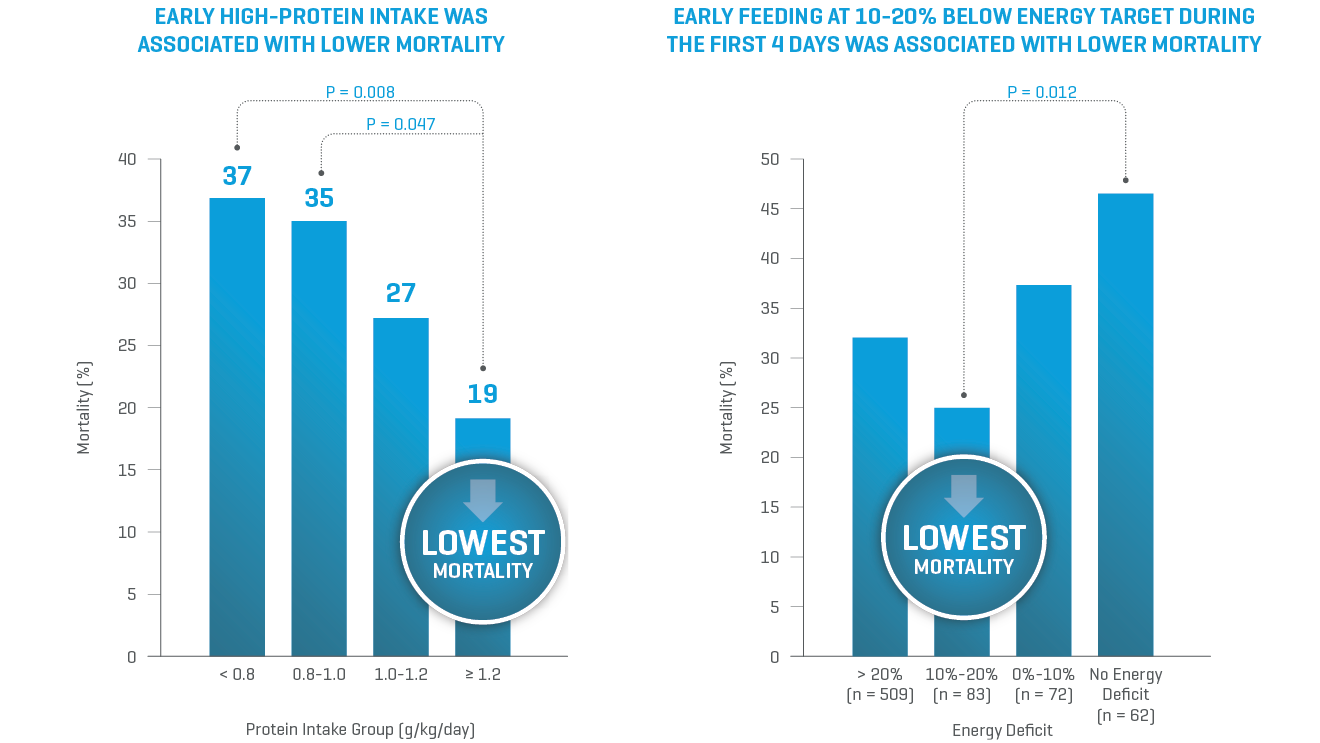
In critically ill patients, high protein intake matters
Timely nutrition that meets protein targets while providing calories 10-20% below the energy target has been associated with lower mortality.14
ESPEN and ASPEN guidelines recommend higher protein content for critically ill patients.1,5 The most frequently recommended protein target for critically ill patients is 1.3-1.5 g/kg/day4,15,16 or even up to 2.0–2.5 g/kg/day.6,15 Baxter offers a range of solutions with high protein content that meets the international guideline recommendations for nutritional support in critically ill patients.
Supplemental Parenteral Nutrition (SPN)
In ICU patients, studies indicate that with the use of enteral nutrition alone, complications may arise from underfeeding because of insufficient nutritional intake.17,18 Individually optimized energy provision with SPN administered between day 4 and day 8 could improve clinical outcomes in severely ill patients in the ICU for whom enteral nutrition (EN) alone is insufficient.17 A systematic review and meta-analysis found that combining EN with SPN improved the protein and energy intakes in critically ill adult patients while decreasing the risk of ICU mortality and nosocomial infections with no adverse effects on other clinical outcomes when initiated before day 8.19 Baxter offers the broadest selection of ready-to-use three-chamber parenteral nutrition (PN) bags to meet the unique nutrition needs of each patient.